We are Niagara Health is a series of stories that celebrates the incredible people working and volunteering in our organization and how they make a difference in the lives of patients and coworkers every day.
After seeing the impact of the COVID-19 pandemic on staff morale in the Intensive Care Unit, Dr. Joyce Lam launched the ICU Survivorship Speaker Series, bringing patients back to the hospital to talk about the care they received and how it has positively impacted them.
Dr. Joyce Lam knows that working in the intensive care unit can be, as the name implies, intense.
The critical care physician and her colleagues in the ICU look after the sickest of the sick, with many of their patients facing insurmountable hurdles in their healthcare journeys. Those dire prognoses are a common enough thread in ICU patient stories that it’s easy for staff to lose sight of the happy endings that have resulted from the extraordinary care they provide.
Dr. Lam is trying to change that. Earlier this summer, she launched an initiative inviting former ICU patients back to the hospital to share their experiences with staff and remind them of the incredible work – and successes – they achieve every day in the ICU.
It’s been especially important since the pandemic when she noticed staff began focusing more on negative outcomes as burnout peaked and morale plummeted.
“I was thinking about some of the amazing cases in the ICU and the patients in the ICU who went back to their regular lives after their ICU stay,” Dr. Lam says. “I wanted staff to hear those stories and see what their efforts amounted to – that it was leading to positive outcomes and good things for the people they helped.”
The first instalment in the ICU Survivorship Speaker Series happened in June when a brother and sister and their family members were invited to share their experiences in critical care and about life since.
The adult siblings were both admitted to the ICU at the same time with COVID-19. While patients may not remember much about their stay in the ICU due to the severity of their condition, the memories and feelings associated with them are often vivid for family.
“We saw so many patients (during the pandemic) that we didn’t think would make it. They leave our ICU and we don’t have any contact afterward. They go home, they go back to their jobs. How has their life changed?"
Compassionate care in action
At the height of the pandemic, when the brother and sister became ill, infection prevention and control rules prevented family from visiting their loved ones in hospital. That made the phone calls from care teams more meaningful to family, who were eager for good news.
During the speaker session in June, the wife of one of the siblings recalled the name of the nurse who phoned to say her husband had recovered to the point he could be taken off his ventilator.
“We stress all the time that families are part of the circle of care and this made it an a-ha moment. This was the only connection the wife had to her husband at the time,” Dr. Lam says. “That nurse was in the room when the wife told that story. They were both in tears when they put together that’s what she was talking about.”
That nurse was Jane, a registered nurse in the ICU at Niagara Health since 2007. When speaking with family on the phone, Jane says she strives to be the calm voice on the other end.
It was an emotional moment to be named by the woman during her talk.

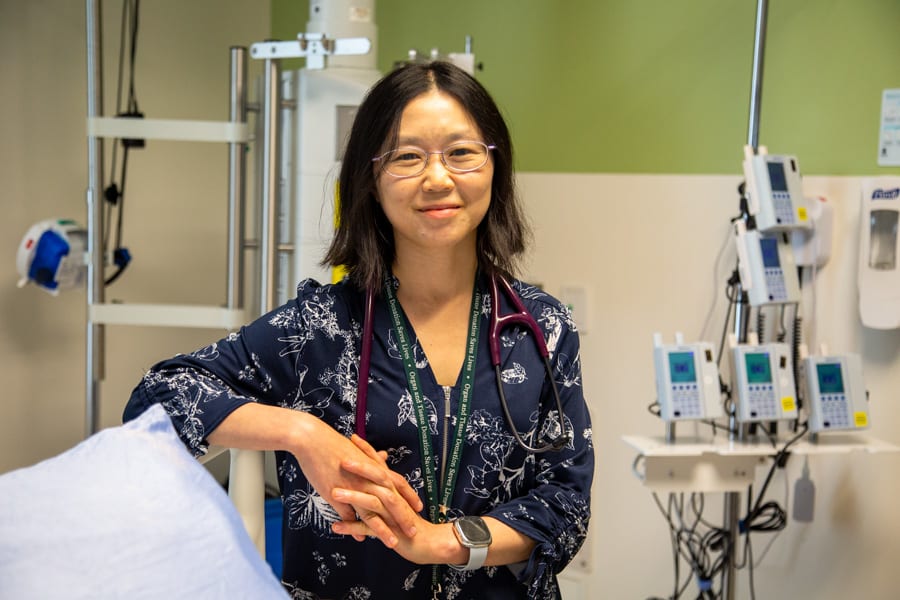
Dr. Joyce Lam at work in the Intensive Care Unit at the Marotta Family Hospital in St. Catharines.
“When patients are as sick as they are, they don’t remember names. They might remember voices but they tend to block things out,” Jane says. “Families remember better. I was happy to bring that excitement to her that day.”
Jane’s family and her coworkers are her usual support systems to help her through the challenging days on the job.
The stress of working in the ICU “comes and goes in waves” and can take a toll, she explains. But everyone rallies around each other during particularly difficult stretches.
Dr. Lam’s ICU Survivorship Speaker Series adds to that support system, Jane notes, especially the chance to hear how people’s stories continue after the chapter in intensive care ends.
“We saw so many patients (during the pandemic) that we didn’t think would make it,” Jane says.
Life after the ICU
“They leave our ICU and we don’t have any contact afterward," Jane adds. "They go home, they go back to their jobs. How has their life changed? In this survivor series, the patient regained everything, mostly. He was able to go back to normal life with his family, which is nice.”
Dr. Lam says patients or their families sometimes reach out to her after leaving the ICU to share the gratitude they feel for care teams. There have been so many patients whose futures were so uncertain that seeing them go on to lead fulfilling lives is incredibly touching.
She plans to have a few of those patients return each year going forward to share their stories with the rest of the ICU team.
“It was incredibly moving to hear this story (in June) because I was taking care of the patients myself and I do distinctly remember how sick (the brother) was. Both patients recovered and have gone back to living their normal lives. It was so great to see and listen to,” Dr. Lam says.
“I say to my colleagues and medical learners that the ICU can be emotionally difficult. We deal with the sickest of the sick and the most critically ill in the hospital. Not all of our patients make it. If we can support them in their darkest moments in life, whatever their outcome might be, patients and their families remember that.”

